The Un-Summit keynote and panel presentations were rich with cutting edge core content. Each session was accompanied by a follow-up discussion via an interactive session designed to expand your understanding of the content through Q&A with the panelists, dialogue, and small group discussions.
Learn more about keynotes and panelists!
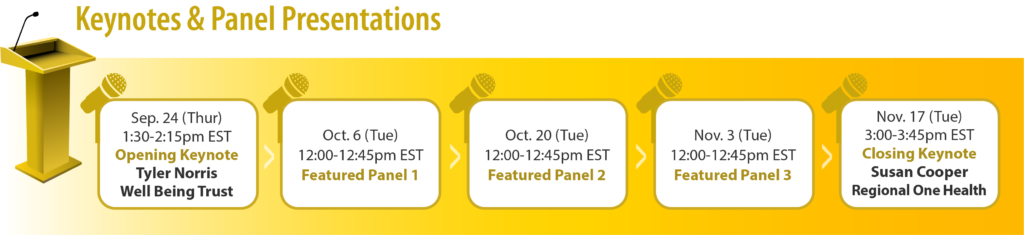
Opening Keynote: Tyler Norris, Chief Executive, Well Being Trust | Creating the Conditions for Health and Well Being
We are at an inflection point in assuring the strength of the systems that underlay the health and well-being of the American public. Even as resources are tight and polarization is rife — there is a clearer understanding of what works and is what is needed to improve population-level outcomes. As multiple concurrent crises and tangled threats persist – how can we lay the foundation for an equitable recovery and resilience over time? Do we want to go ‘back to normal’ and who benefits/loses from that; or is the vision something quite different? How can we shape dose-sufficient investments in community health and well-being in these unprecedented times. To become a healthy, thriving community, multiple vital conditions must be in place for all to access. These vital conditions, though in part supported by national work, require investments, policy and practice changes at the local level. Join Tyler Norris to learn how deliberate engagement of communities via authentic partnerships can result in improved health outcomes.
Panel 1 | Partnerships in the Community: Imperative to Keeping the PACE
Rising rates of opioid-related deaths and homelessness led the Philadelphia Department of Behavioral Health and Intellectual disAbility Services (DBHIDS) to take action. Developed within their PACE Strategic Framework (Prioritizing to Address our Changing Environment, released in 2018), DBHIDS launched a spectrum of services within a population health framework, including AR2, a partnership between DBHIDS, the Philadelphia FIRE Department, and the Philadelphia Department of Public Health, as well as the Community Wellness Engagement Unit (CWEU), a team designed to increase and enhance access to behavioral health services across city council districts through Philadelphia. CWEU operates from the premise that communities don’t only have challenges; they also have assets. Its assets are found in community residents, schools, faith communities, and other stakeholders already doing good work. CWEU believes that their work should be guided by the priorities identified by the community and partnerships are a hallmark to everything DBHIDS does, particularly as it relates to the opioid epidemic.
Panel 2 | The Beginning of the End: Leveraging Partnerships, Data, and Lived Expertise to Effectively End Youth Homelessness in Austin, Texas
As part of the broader federal strategy to end homelessness in the United States, the Youth Homelessness Demonstration Program (YHDP) was designed to support the development of coordinated community responses to effectively end youth homelessness by 2020—that is, to measurably demonstrate that youth homelessness in the community is “rare, brief, and non-recurring.” Selected communities are responsible for introducing innovative housing programs, addressing systemic causes of youth homelessness, and providing wraparound support services to prevent future homelessness. Since 2017, key stakeholders in Austin—including youth with lived experience of homelessness, members of the homelessness response system, and representatives from juvenile justice, child welfare, and local school districts, among others—worked together to develop three new programs, grounded in best practices, guided by data, and informed by consumer feedback: rapid rehousing, prevention and diversion, and a housing navigation shelter. The YHDP is designed to be a community-wide collaboration to ensure its long-term sustainability. Given the disproportionately higher rates of systems involvement observed among youth experiencing homelessness in Austin (76% relative to 55% nationwide), coupled with the lack of affordable housing, the formation of such partnerships is critical for stemming the inflow into homelessness among youth in our community. As a result of these efforts thus far, from January 2019 to January 2020, Austin has experienced a 28% decline in youth homelessness. The community is committed to bringing youth homeless to functional zero by 2021.
Panel 3 | Douglas County Mental Health Initiative: A Unique Community Partnership
The Douglas County Mental Health Initiative (DCMHI) launched in June of 2014 following a series of tragic events in the community. DCMHI sought to address unmet mental health needs, connect people to mental health services, and prevent those in need from falling through the cracks of the mental health system. After using process mapping to identify existing gaps in the delivery system and to prioritize programs, a collective impact approach was adopted as a framework to support implementation, partner engagement, evaluation and ongoing system sustainability. From this work the Community Response Team (CRT) program was designed. The purpose was to connect residents to the most appropriate care to meet their needs, reduce emergency department visits, and avoid arrests. DCMHI operates on the premise that a collective impact approach, involving all relevant stakeholders and viewpoints, is vital to success and achieving their vision for an integrated community-based mental health care delivery system.
Closing Keynote: Susan R. Cooper, Chief Integration and Senior Vice President, Regional One Health | Moving the Needle – Building Authentic Community Partnerships Together as ONE
One Health is a program designed to meet the needs of our uninsured, medically and socially complex patients. The goal of the program is to improve the health of our most vulnerable, while bending the cost curve. Complex patients comprise a small, heterogeneous group of individuals who frequently cycle through multiple systems (healthcare, behavioral, social, correctional), but do not receive any lasting benefit from the interactions. Care is often fragmented and systems are rarely designed to meet the needs of the most complex. Hospitals alone are insufficient to meet the complex needs of these patients. A new mindset for building authentic partnerships was required. The team built authentic relationships with cross-sector community partners based on data and trust. New tools were developed and implemented for community asset mapping, model design, and data collection, which led to the creation of a new ecosystem of care inclusive of healthcare, behavioral health, and social services. Additionally, new methods of cross sector collaboration were introduced. Over the course of 27 months, 430 individuals were enrolled. Improved outcomes were achieved in health, housing, utilization, cost, benefits, food security, and self-sufficiency.